The HIFE Program has been evaluated in several studies in varying settings and populations, for example people with dementia, stroke or hip fracture. A short description, including references, is presented below.
HIFE in nursing homes
The Frail Older People Activity and Nutrition (FOPANU) Study
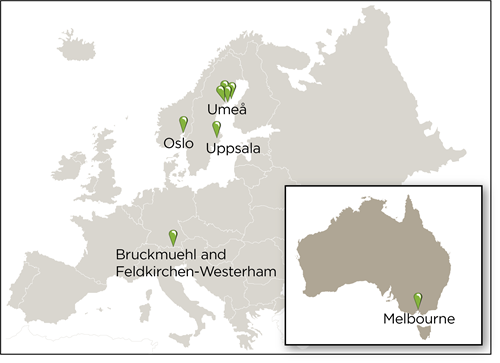
This randomized controlled trial (RCT) included 191 older people living in nursing homes in Umeå, Sweden. The participants were 65 years or over (mean age 85 years) and 100 of them were diagnosed with dementia (Rosendahl et al. 2006). Participants were randomized to either exercise (n=91) according to the HIFE Program or a seated control activity (n=100). For both activities, five sessions (of approximately 45 min each) were held per fortnight for 3 months. Attendance was 72% for the exercise group and 70% for the control group. No adverse events, that led to a manifest injury or disease, occurred during the exercise sessions (Littbrand et al. 2006). The results from the FOPANU Study showed positive effects of the exercise on self-paced gait speed and reduced decline in Activities of Daily Living (ADL) related to indoor mobility, both at 3 months (directly after intervention period) and at 6 months, when compared to the control activity (Rosendahl et al. 2006, Littbrand et al. 2009). At 6 months, positive effects of exercise were also seen in leg strength and balance (Rosendahl et al. 2006). A reduction in falls was seen in the exercise group among participants who improved their balance (Rosendahl et al. 2008). There were negative effects of exercise on muscle mass and body weight at 6 months (Carlsson et al. 2011).
Among people with dementia, the study showed that the exercise program had positive effects regarding reduced decline in overall ADL performance and improved well-being when compared to the control group (Littbrand et al. 2009, Conradsson et al. 2010). Further, neither the applicability of the program (attendance, exercise intensity, adverse events) nor the effect on balance differed between persons with dementia and those without (Littbrand et al. 2006 and 2011).
More participants in the exercise group prioritized the exercise above other activities, according to results from interview questionnaires (Lindelöf et al. 2013). They also reported that, as a result of the exercise, they felt less tired and perceived improvements in lower-limb strength, balance, and safety and security when mobile, to a significantly greater degree than the participants in the control group. Findings from interviews with participants in the exercise group showed, for example, that they believed in positive effects and had a strong will to be active in order to avoid decreased capacity (Lindelöf et al. 2012). Further, the participants told of improvements in body and soul and that exercising in groups created a sense of togetherness.
The Umeå Dementia and Exercise (UMDEX) Study
This RCT included 186 older people aged 65 years or over (mean age 85 years) with diagnosed dementia and living in nursing homes in Umeå, Sweden (Toots et al. 2016). Participants were randomized to either exercise (n=93) according to the HIFE Program or a seated control activity (n=93). For both activities, five sessions (approximately 45 min each) were held per fortnight over 4 months. The results from the UMDEX Study showed that exercise slowed decline in ADL independence and improved balance when compared to the control group, both at 4 months (directly after the intervention period) and at 7 months, albeit only in participants with non-Alzheimer’s dementia (Toots et al. 2016). Exercise had positive effects on self-paced forward gait speed, compared to the control group, when tested unsupported but not when walking aids or a minimum amount of living support were used in the test (Toots et al. 2017a). There were no overall exercise effects on backwards walking speed, bur the results indicated positive effects in participants who habitually walked unaided (Toots et al. 2021).
No between-group effects were found on cognition or depressive symptoms (Boström et al. 2016, Toots et al. 2017b). Participants in both the exercise and control groups with higher levels of depressive symptoms at baseline showed significant reductions in depressive symptoms at 4 and 7 months (Boström et al. 2016). Regarding falls, no difference in fall rate between groups at 6 or 12 months were found (Toots et al 2019). Participants in the exercise group were less likely to sustain moderate/serious fall-related injuries at 12-month follow-up.
Attendance was 73% in the exercise group and 70% in the control group. Motivation was high or very high during 61% of attended sessions in the exercise group and 63% in the social activity group (Sondell et al. 2018). The adverse events in the exercise group were all minor and temporary (Sondell et al. 2019a). Low motivation was the most common barrier for attendance in the exercise group. Of medical conditions, only behavioral and psychological symptoms of dementia, including apathy, were negatively associated with attendance (Sondell et al. 2019a). Twenty-nine (36%) of the participants in the exercise group were categorized as responders (a ≥5-point increase in the Berg Balance Scale). Predicting balance exercise response based on applicability and motivation seemed not to be possible (Sondell et al 2019b).
According to interviews with participants in the exercise group the intense exercise was perceived as challenging but achievable since it was individually tailored and adapted (Lindelöf et al. 2017). Participants described that exercising gave them pleasure, brought improvements in mental and bodily strength, awakened memories of previous physical activities and that they rediscovered bodily capabilities.
From interviews with the leaders of the exercise groups, the authors concluded that a continuous iterative process of building on existing knowledge, sharing and reflecting, being alert to any alterations needed for individuals that day, communication skills (both with residents and staff) and building a relationship and trust with residents are all important for effective delivery of high intensity functional exercise to older people living with dementia in care settings (Fjellman-Wiklund et al. 2016).
The Exercise and Dementia (EXDEM) Study
This RCT included 170 people aged 55 years or over (mean age 87 years) with dementia and living in nursing homes in and around Oslo, Norway (Telenius et al. 2015a). Participants were randomized to either exercise according to the HIFE Program (n=87) or a control activity (n=83), both had sessions twice a week for 3 months. The attendance rate was 75% for the exercise group and 69% for the control group. No adverse effect of exercise occurred. Results from the EXDEM Study showed positive exercise effects on balance at 3 months (directly after intervention period) and at 6 months compared to the control group (Telenius et al. 2015a and 2015b). Regarding Behavioural and Psychological Symtoms of Dementia (BPSD), the level of apathy and agitation was lower in the exercise group at 3 and 6 months, respectively, compared to the control group (Telenius et al. 2015a and 2015b). Five overreaching and interrelated themes emerged from interviews with participants in a pilot study for the RCT; “Being invested in,” “Relationships facilitate exercise participation,” “Exercise revives the body, increases independence and improves self-esteem”, and “Physical activity is a basic human necessity—use it or lose it!” (Olsen et al. 2015).
Feasibility of HIFE in nursing homes in Germany
This feasibility study included 16 participants, aged 75 to 96 years, in two nursing homes in Bruckmuehl and Feldkirchen-Westerham, Germany (Kastner et al. 2017). Exercise according to the HIFE Program was performed in the two groups, one at each nursing home, twice a week for 10 weeks. No serious adverse events appeared and the attendance was high, 14 of the 16 participants participated in at least 75% of the exercise sessions. Further, acceptance of the HIFE Program by both the managing director and nursing staff were very good. Static balance, functional leg strength, and self-paced gait speed improved significantly, but not maximal gait speed or Timed Up and Go (TUG).
Rehabilitation in hospital and subsequent home rehabilitation
Effects of a High Intensity Functional Exercise (HIFE) Group on Mobility in Older People in the Sub-Acute Setting
This RCT included 468 people aged 65 years or over (mean age 84 years) and admitted to Geriatric Evaluation and Management wards at a rehabilitation hospital in Melbourne, Australia (Raymond et al. 2017). Participants were randomized to a HIFE group three times a week and individual physiotherapy sessions twice a week (n=236) or were offered individual physiotherapy sessions five times per week (n=232). No adverse events were registered as related to participation in the trial. There were no between-group differences either in mobility, assessed by the Elderly Mobility Scale, or in length of stay or discharge destination. Significantly more participants in the HIFE group improved their balance, assessed by the Berg Balance Scale, by a minimal clinical detectable difference. Authors concluded that replacing several individual sessions with the HIFE group may improve mobility similarly to individual sessions alone, without affecting discharge destination or length of stay, and that therapists were more efficient utilized in group exercise.
Geriatric interdisciplinary home rehabilitation for older people with hip fracture
This RCT included 205 people aged 70 or over (mean age 83 years) operated for a hip fracture at a hospital in Umeå, Sweden (Karlsson et al. 2016). Sixty-nine percent lived in ordinary housing and 31% in nursing home. Participants were randomized either to geriatric interdisciplinary home rehabilitation or conventional geriatric care and rehabilitation. Home rehabilitation that was individually designed and carried out by an interdisciplinary team for a maximum of 10 weeks and aimed at early hospital discharge and continuation of rehabilitation in their homes. Special priority was given to prevention of falls, independence in daily activities, and walking ability both indoors and outdoors. The physiotherapy intervention focused on walking ability indoors and outdoors, and functional strength and balance training according to the HIFE Program. Results showed that the median postoperative length of stay in the geriatric ward was significantly shorter for the home rehabilitation group, median 17 days compared to 23 days in the control group (Karlsson et al. 2016). No significant differences between the groups were observed in walking ability, use of walking device, gait speed, or independence in ADL at the 3- and 12-month follow-up (Karlsson et al. 2016 and 2020a). Further, no significant differences were found in numbers of complications, readmissions, and total days spent in hospital after discharge during a 12-month follow-up period (Berggren et al. 2019). The effects of geriatric interdisciplinary home rehabilitation versus in-hospital geriatric care did not differ significantly between participants with and without dementia, in regards to falls, performance in ADL, or walking ability (Karlsson et al. 2020b).
HIFE with community-dwelling people
Effect of Intensified Physical Activity for Patients with Stroke
This RCT included 67 people with stroke that were between 65 and 85 years of age (mean age 73 years) and living in the community in the Uppsala region, Sweden (Vahlberg et al. 2017a). They had had an initial or recurrent stroke at least 1 year before inclusion. Participants were randomized to either exercise according to the HIFE Program combined with motivational group discussions twice weekly for 3 months (n=34) or a usual care control group (n=33). The results from the study showed positive effects of exercise on balance and performance on six-minute walking test at 3 months (directly after the intervention period) and on self-paced walking speed over 10 meters at 3, 6, and 15 months, when compared to the control group (Vahlberg et al. 2017a). The intervention group reduced fat mass at 3 months, in comparison with the control group (Vahlberg et al 2017b).
Benefits of a High-Intensive Exercise Program after Stroke
This RCT included 34 people with stroke that were over 55 years of age (mean age 79 years) and living in the community, including in the form of senior housing, in and around Umeå, Sweden (Holmgren et al 2010a). They had had an initial or recurrent stroke 3-6 months before inclusion. Participants were randomized to either exercise according to the HIFE Program combined with implementation of the same exercises into everyday life activities, e.g. walking outdoors or sweeping the yard (n=15) or to a control group (n=19). Exercise sessions (of approximately 45 min each) took place six times each week, divided over three days, in total of 30 exercise sessions over 5 weeks. In addition, the exercise group participated in an educational discussion session one day each week, a total of five educational sessions over 5 weeks, about the increased risks of complications, such as falls, after stroke The control group also met once a week for educational sessions during the 5-week period. These group discussions concerned communication difficulties, fatigue, depressive symptoms, mood swings, personality changes, and dysphagia. The results from the study showed positive effects for the intervention group regarding fear of falling directly after intervention and at 3 months post-intervention, as well as on ADL at 6 months, compared with the control group (Holmgren et al. 2010a). There were significant differences between the groups for parts of the SF-36 used for evaluating health-related quality of life at 3 months post-intervention in, in favor of the control group (Holmgren et al. 2010b).
Effects of a multicomponent high intensity exercise program in older adults with or at risk of mobility disability after discharge from hospital
This RCT included 89 people aged 65 or over (mean age 78 years) with or at risk of mobility disability after discharge from a medical ward at the general hospital in Oslo, Norway (Sunde et al. 2020). Baseline testing was conducted median 49 days after discharge, before randomization to an intervention group (n=45) or a control group (n=44). The intervention group performed a group-based high intensity exercise program, twice a week for four to five months, maximum 32 sessions or 5 months. The intervention was based on the Norwegian Ullevaal model and the eight predetermined exercises from the HIFE Program. It was led by one or two physiotherapists, in groups of 2–10 participants. Both the intervention and control groups were instructed in a home-based exercise program and were encouraged to exercise according to World Health Organization’s recommendations for physical activity in older people. At 4 months, 29 participants in the exercise group and 30 participants in the control group were followed-up. The mean attendance for those followed-up in the exercise group was 25.5 sessions. The primary outcome, physical performance, was measured by the Short Physical Performance Battery (SPPB). Secondary outcomes were 6-min walk test (6MWT), Berg Balance Scale (BBS), grip strength, Body Mass Index (BMI), and HRQOL (the Short-Form 36 Health Survey (SF-36)). Intention-to-treat analysis showed that the intervention group improved their functional capacity (6MWT) and the physical component summary of SF-36 significantly compared to the control group. No further between-group differences in change from baseline to 4 months follow-up were found.
References
Berggren M, Karlsson Å, Lindelöf N, Englund U, Olofsson B, Nordström P, Gustafson Y, Stenvall M (2019). Effects of geriatric interdisciplinary home rehabilitation on complications and readmissions after hip fracture: a randomized controlled trial. Clin Rehabil; 33:64-73.
Boström G, Conradsson M, Hörnsten C, Rosendahl E, Lindelöf N, Holmberg H, Nordström P, Gustafson Y, Littbrand H (2016). Effects of a high-intensity functional exercise program on depressive symptoms among people with dementia in residential care: a randomized controlled trial. Int J Geriatr Psychiatry; 31:868-78.
Carlsson M, Littbrand H, Gustafson Y, Lundin-Olsson L, Lindelöf N, Rosendahl E, Håglin L (2011). Effects of high-intensity exercise and protein supplement on muscle mass in ADL dependent older people with and without malnutrition – a randomized controlled trial. J Nutr Health Aging; 15:554-60.
Conradsson M, Littbrand H, Lindelöf N, Gustafson Y, Rosendahl E (2010). Effects of a high-intensity functional exercise program on depressive symptoms and psychological wellbeing among older people living in residential care facilities: a randomized controlled trial. Aging Ment Health; 14:565-76.
Fjellman-Wiklund A, Nordin E, Skelton DA, Lundin-Olsson L (2016). Reach the person behind the dementia – Physical Therapists’ reflections and strategies when composing physical training. PLoS One; 11(12):e0166686.
Holmgren E, Lindström B, Gosman-Hedström G, Nyberg L, Wester P (2010a). What is the benefit of a high intensive exercise program? A randomized controlled trial. Adv Physiother; 12:115-24.
Holmgren E, Gosman-Hedström G, Lindström B, Wester P (2010b). What is the benefit of a high-intensive exercise program on health-related quality of life and depression after stroke? A randomized controlled trial. Adv Physiother; 12:125-33.
Karlsson Å, Berggren M, Gustafson Y, Olofsson B, Lindelöf N, Stenvall M (2016). Effects of geriatric interdisciplinary home rehabilitation on walking ability and length of hospital stay after hip fracture: a randomized controlled trial. J Am Med Dir Assoc; 17:464.e9-15.
Karlsson Å, Lindelöf N, Olofsson B, Berggren M, Gustafson Y, Nordström P, Stenvall M (2020a). Effects of geriatric interdisciplinary home rehabilitation on independence in activities of daily living in older people with hip fracture: a randomized controlled trial. Arch Phys Med Rehabil; 101:571-8.
Karlsson Å, Berggren M, Olofsson B, Stenvall M, Gustafson Y, Nordström P, Lindelöf N (2020b). Geriatric interdisciplinary home rehabilitation after hip fracture in people with dementia – a subgroup analysis of a randomized controlled trial. Clin Interv Aging; 15:1575–86.
Kastner S, Becker C, Lindemann U (2017). High Intensity Functional Exercise (HIFE) Training Machbarkeitsstudie [Article in German, abstract in English also]. Physioscience; 13:109–16.
Lindelöf N, Karlsson S, Lundman B. Experiences of a high-intensity functional exercise programme among older people dependent in activities of daily living (2012). Physiother Theory Pract; 28:307-16.
Lindelöf N, Rosendahl E, Gustafsson S, Nygaard J, Gustafson Y, Nyberg L (2013). Perceptions of participating in high-intensity functional exercise among older people dependent in activities of daily living (ADL). Arch Gerontol Geriatr; 57:369-76.
Lindelöf N, Lundin-Olsson L, Skelton DA, Lundman B, Rosendahl E (2017). Experiences of older people with dementia participating in a high-intensity functional exercise program in nursing homes: “While it’s tough, it’s useful”. PLoS One; 12(11):e0188225.
Littbrand H, Rosendahl E, Lindelöf N, Lundin-Olsson L, Gustafson Y, Nyberg L (2006). A high-intensity functional weight-bearing exercise program for older people dependent in activities of daily living and living in residential care facilities: evaluation of the applicability with focus on cognitive function. Phys Ther; 86:489-98.
Littbrand H, Lundin-Olsson L, Gustafson Y, Rosendahl E (2009). The effect of a high-intensity functional exercise program on activities of daily living: a randomized controlled trial in residential care facilities. J Am Geriatr Soc; 57:1741-9.
Littbrand H, Carlsson M, Lundin-Olsson L, Lindelöf N, Håglin L, Gustafson Y, Rosendahl E (2011). The effect of a high-intensity functional exercise program on physical function: Preplanned subgroup analyses of a randomized controlled trial in residential care facilities. J Am Ger Soc; 59:1274-82.
Olsen CF, Telenius EW, Engedal K, Bergland A (2015). Increased self-efficacy: the experience of high-intensity exercise of nursing home residents with dementia – a qualitative study. BMC Health Serv Res; 15:379.
Raymond MJ, Jeffs KJ, Winter A, Soh SE, Hunter P, Holland AE (2017). The effects of a high-intensity functional exercise group on clinical outcomes in hospitalised older adults: an assessor-blinded, randomised-controlled trial. Age Ageing; 46:208-13.
Rosendahl E, Lindelöf N, Littbrand H, Yifter-Lindgren E, Lundin-Olsson L, Håglin L, Gustafson Y, Nyberg L (2006). High-intensity functional exercise program and protein-enriched energy supplement for older persons dependent in activities of daily living; a randomised controlled trial. Aust J Physiother; 52:105-13.
Rosendahl E, Gustafson Y, Nordin E, Lundin-Olsson L, Nyberg L (2008). A randomized controlled trial of fall prevention by a high-intensity functional exercise program for older people living in residential care facilities. Aging Clin Exp Res; 20:67-75.
Sondell A, Rosendahl E, Sommar JN, Littbrand H, Lundin-Olsson L, Lindelöf N (2018). Motivation to participate in high-intensity functional exercise compared with a social activity in older people with dementia in nursing homes. PLoS One; 13:e0206899.
Sondell A, Rosendahl E, Gustafson Y, Lindelöf N, Littbrand H (2019a). The applicability of a high-intensity functional exercise program among ölder people with dementia living in nursing homes. J Geriatr Phys Ther; 42:E16-24.
Sondell A, Littbrand H, Holmberg H, Lindelöf N, Rosendahl E (2019b). Is the effect of a high-intensity functional exercise program on functional balance influenced by applicability and motivation among older people with dementia? J Nutr Health Aging 2019: 23:1011-20.
Sunde S, Hesseberg K, Skelton DA, Ranhoff AH, Pripp AH, Aarønæs M, Brovold T (2020). Effects of a multicomponent high intensity exercise program on physical function and health-related quality of life in older adults with or at risk of mobility disability after discharge from hospital: a randomised controlled trial. BMC Geriatr; 20:464.
Telenius EW, Engedal K, Bergland A (2015a). Effect of a high-intensity exercise program on physical function and mental health in nursing home residents with dementia: an assessor blinded randomized controlled trial. PLoS One; 10(5):e0126102.
Telenius EW, Engedal K, Bergland A (2015b). Long-term effects of a 12 weeks high-intensity functional exercise program on physical function and mental health in nursing home residents with dementia: a single blinded randomized controlled trial. BMC Geriatr; 15:158.
Toots A, Littbrand H, Lindelöf N, Wiklund R, Holmberg H, Nordström P, Lundin-Olsson L, Gustafson Y, Rosendahl E (2016). Effects of a high-intensity functional exercise program on dependence in activities of daily living and balance in older adults with dementia. J Am Geriatr Soc; 64:55-64.
Toots A, Littbrand H, Holmberg H, Nordström P, Lundin-Olsson L, Gustafson Y, Rosendahl E (2017a). Walking aids moderate exercise effects on gait speed in people with dementia; a randomized controlled trial. J Am Med Dir Assoc; 18:227-33.
Toots A, Littbrand H, Boström G, Hörnsten C, Holmberg H, Lundin-Olsson L, Lindelöf N, Nordström P, Gustafson Y, Rosendahl E (2017b). Exercise on cognitive function in older people with dementia: A randomized controlled trial. J Alzheimers Dis; 60:323-32.
Toots A, Wiklund R, Littbrand H, Nordin E, Nordström P, Lundin-Olsson L, Gustafson Y, Rosendahl E (2019). The effects of exercise on falls in older people with dementia living in nursing homes: a randomized controlled trial. J Am Med Dir Assoc; 20:835-42.
Toots A, Lundin-Olsson L, Nordström P, Gustafson Y, Rosendahl E (2021). Exercise effects on backward walking speed in people with dementia: A randomized controlled trial. Gait Posture: 85:65-70.
Vahlberg B, Cederholm T, Lindmark B, Zetterberg L, Hellström K (2017a). Short-term and long-term effects of a progressive resistance and balance exercise program in individuals with chronic stroke: a randomized controlled trial. Disabil Rehabil; 39:1615-22.
Vahlberg B, Lindmark B, Zetterberg L, Hellström K, Cederholm T (2017b). Body composition and physical function after progressive resistance and balance training among older adults after stroke: an exploratory randomized controlled trial. Disabil Rehabil; 39:1207-14.